
Blog
Expecting – and Getting – More for Our Healthcare Dollars
By Katie Higgins
In any industry, it takes the changemakers to go out on a limb, make the bold move and pull everyone else along. In healthcare, we have seen large employers – with diverse populations – be the changemakers. Some have been doing it for a decade now, experiencing the value of Advanced Primary Health, and the benefits of lower overall costs and better health outcomes for their employees.
So what is it going to take to get the masses on board?
To start with, let’s take a look at one of the systemic – and potentially worsening – problems with healthcare: The sticker shock that pretty much anyone who’s been to the doctor – for themselves or a loved one – can relate to.
Paying for Piecework
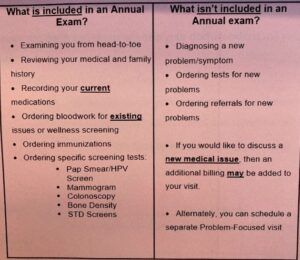
Here is a true story. Not long ago, I scheduled an annual wellness exam with my community Primary Care doctor. I wanted to get on top of critical health screenings and have that one consistent person to go to when sick or have a concern vs always running to urgent care. That vision wasn’t realized. When I showed up for my visit, I was handed two waivers to sign. The first stated that my visit would cost $320 and that while this cost would be covered by my insurance company (less my copay), if I scheduled a second well visit less than 365 days out, I would be responsible for the $320. The second waiver that I signed looked like this:
Got it. This well visit was not intended to focus on my whole health… just checking the box on my health as we know it today. Lasting less than 15 minutes, the entire experience left me wondering: what was the point? The constraints allowed for no conversation at all; just a cursory review of the basics and on to the next patient. Was she a bad doctor? Certainly not. Just a doctor practicing in the face of the real culprit – a payment system that views patients as parts and pieces to be serviced, not as whole people seeking to be well. For me, this was one of the clearest examples of how FFS directly interferes with trusted physician relationship building and the best care delivery.
The Point of No Return
Here’s the hard truth that is staring down every single employer – if healthcare costs continue to increase at the same rate, in a decade many employers will not be able to afford this key benefit. In fact, If we look at the average premium for family coverage, we see that it has increased 22% over the last five years and 47% over the last ten years. (2021 Employer Health Benefits Survey)
So how is a system that’s arguably been broken for so long going to get fixed by crunch time? It has to be an approach that measurably improves wellbeing and outcomes actually lowers costs and keeps employees healthy.
Taking Accountability, Creating Trust
First, accessible, affordable and outcomes – focused quality healthcare does exist. You just have to look for it and demand it.
At Crossover, we’re creating a world where the cost of healthcare doesn’t drive coverage off a cliff. We do this by controlling cost through an integrated experience and a care team that surrounds the patient and sets goals. And by offering care that’s comprehensive and inclusive of mental health, physical health, health coaching and care navigation – delivered by a trusted, accountable team. And at a deeper, underlying level, we do this by measuring our care progress along the way so that we can produce tangible care outcomes consistently.
Then data is used to enroll members in the programs or services that are relevant to their health concerns and gaps in care. As we offer care to the member, we work with our clients to uncover clinical insights related to the health trends of their employee populations and leverage this data to brainstorm additional resources and benefits to improve the overall health trajectory of their employees. And employers are realizing that outcomes and patient engagement, not just utilization, are the key to controlling the out-of-control costs of healthcare.
Last, but definitely not least, providing flexible access to care is also key. Our hybrid offering – which wraps our national virtual care network around the onsite and nearsite health clinic access – provides members with choice. It allows employers to actively manage healthcare delivery costs and provide high quality healthcare to all employees; the best care anywhere.
So now is the time – more so than ever – for every individual and every employer to be the changemakers in this industry by expecting more and thinking differently about health delivery. With healthcare costs rising exponentially, employers – the true payers for over 150 million Americans – are losing out from a FFS payment model that works at cross purposes to the quadruple aim. It’s time for employers to hold their healthcare partners accountable for outcomes, not just visit volume and services. It’s time to demand an integrated care team that replaces today’s disconnected silos. And it’s time for employees to choose how they want to interact with their care team – in person, virtually or asynchronously. And all this should be done with the currency of trust.
___
About the Author

As Chief Revenue Officer of Crossover Health, Katie is passionate about creating a healthcare model that achieves easier access, greater affordability, and reliable outcomes for all individuals. She has built and led teams that provide outstanding client service and innovative partnership opportunities for healthcare companies. Keys to her success have been identifying and cultivating great talent, and creating strong team camaraderie, which combine to help achieve ambitious business objectives with clients primarily in the provider market. Katie is also known for her commitment to cultivating rising female talent—a critical need in the healthcare industry.